Opening Plenary examines advances in decoding cancer complexity, future research directions
Cancer is a complex constellation of diseases driven by thousands of distinct cancer genes and oncogenic somatic mutations. Normal cells also harbor numerous mutations, yet do not give rise to cancer—or do not appear to give rise to cancer.
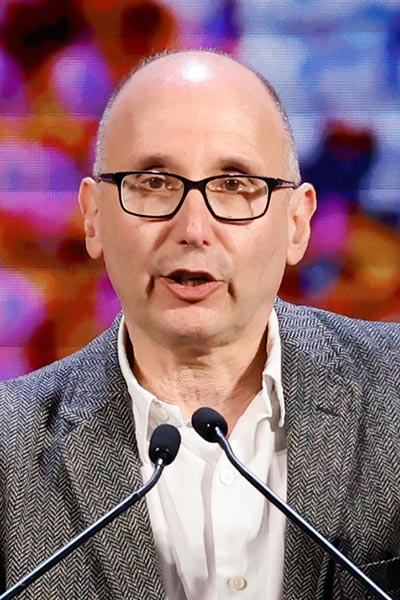
“Mutagenesis is a ubiquitous biological process,” said Michael R. Stratton, MBBS, PhD, FAACR, Wellcome Trust Sanger Institute, Cambridge, United Kingdom. “Cancer cells spend a significant amount of time looking like normal cells. Looking at mutagenesis in normal and cancerous cells can help elucidate the origins of cancer.”
Stratton was the first presenter in the Opening Plenary Session of the AACR Annual Meeting 2022 on Sunday, April 10. The session, Decoding Cancer Complexity, Integrating Science, Transforming Patient Outcomes, featured five state-of-the-art scientific presentations and a special lecture on the future of cancer research by Charles L. Sawyers, MD, FAACR, Memorial Sloan Kettering Cancer Center. The plenary can be viewed on the virtual platform by registered meeting participants through July 13, 2022.
Stratton discussed the mechanisms by which inherited DNA repair defects can affect the pathogenesis of cancer. Normal cells in colorectal crypts accumulate about 50 somatic mutations during each year of life, he explained. Each crypt is derived from a single stem cell and composed of 1,000 to 2,000 identical cells. Each crypt is a unique clone with a unique mutational history.
But even though crypts accumulate a new somatic mutation every week, only about one mutation a year involves a structural deletion or insertion, Stratton explained. Colorectal cancer (CRC) cells carry a mutational burden about seven times higher—350 mutations per year.
Inherited cancer syndromes also have elevated mutational rates, which vary by syndrome. Some syndromes have very high rates of mutation, others less so.
“Every cell in every crypt carries a mutational burden,” Stratton said. “It turns out that normal human cells are pretty tolerant of mutations, which raises a lot of questions.”

Human cells also evolve in response to genomic and epigenomic alterations, and many of those alterations are heritable. Variation in DNA, methylation, and other features can affect cellular reproduction and survival, noted Franziska Michor, PhD, Dana-Farber Cancer Institute and Harvard University.
“Tumor evolution might include signals to ignore cell death, to increase proliferation, to change state, and more,” she said.
Most tumors that are treated eventually develop resistance, in part because cancer treatments are not designed to minimize the development of resistance, Michor said. Redesigning treatment strategies that prevent or minimize resistance might improve patient outcomes.
Working with lung adenocarcinomas and resistance to tyrosine kinase inhibitors, Michor’s lab developed an evolutionary model of resistance coupled with pharmacokinetics to optimize dosing strategies to maximize clinical efficacy and minimize treatment resistance.
“This modeling platform can be extended to identify personalized treatment strategies to slow evolution of treatment resistance,” Michor said. “Nothing in cancer biology makes sense unless seen through the lens of evolution.”

Examining the human microbiome is another approach to understanding cancer pathogenesis. About 20 percent of all cancers are associated with infection, said Jason M. Crawford, PhD, Yale University, and many of those infections are caused by organisms resident in the microbiome.
Bacteria in the microbiome are capable of regulating host response through inflammation, signal transduction, DNA damage, or other mechanisms. Macrophages and other immune components of the host system, and the immunometabolism—the intersection between immunology and metabolism—are similarly able to regulate microbiota.
“The microbiome is a new frontier in chemical ecology,” Crawford said. “The host-microbe interface is a complex interplay of molecules produced by the host and the microbiome, all of which can interact in this diverse ecosystem.”
E. coli resident in the gut can produce multiple chemical entities, he continued. One of them, colibactin, is present in 50 percent to 67 percent of CRC patients compared to 20 percent of healthy individuals. About 10 percent of CRC patients have driver mutations that are consistent with colibactin damage to DNA and DNA damage repair pathways.
“Genotoxicity, by way of DNA damage, is consistent with cancer risk and varies by metabolism,” Crawford said. “The amount of genotoxic bacteria in our gut is much larger than we had previously appreciated.”

The role of diet is also a factor in tumor metabolism and tumor progression. It has long been clear that obesity increases risk in many cancer types.
“Tumors do not exist in isolation,” said Marcia C. Haigis, PhD, Harvard Medical School. “They exist in the environment with multiple other factors and cells. Systemic metabolism affects cancer progression and cancers alter nutrient use in the host.”
Cancer cells are voracious, consuming enormous quantities of proteins, sugars, and fats to fuel growth, proliferation, stress defense, signaling, and other functions, she explained. T cells also have potent metabolic demands. Interfering with normal metabolic pathways, as tumor cells can do by depleting nutrients in the tumor microenvironment (TME), can alter immune cell function and trajectory.
T-cell function depends on mitochondrial metabolism, Haigis explained, and tumors downregulate prolyl hydroxylase domain enzyme (PHD)3, which increases fat oxidation and depletes fatty acids in the TME. Reducing fatty acids starves CD8+ T cells and reduces antitumor activity.
At the same time, obesity reduces the proportion of intratumoral CD8+ T cells by further depleting fatty acids from in the TME. In mouse models, overexpressing PHD3 is sufficient to reduce tumor growth even on a high-fat diet.
In CRC patients, tumors that are PHD3-low are immunologically cold, while tumors high in PHD3 are immunologically hot.
“Diet-induced obesity causes profound changes in T-cell function,” Haigis said. “We are able to restore T-cell function by restoring PHD3 function in tumor cells. We need to identify other pathways and immune cell types that are important during obesity, as well as the impact of age and other systemic states of cellular and molecular mechanisms in the TME.”
Early detection through improved cancer screening is another opportunity.

“Earlier detection can make a significant difference in patient outcomes,” said Nickolas Papadopoulos, PhD, Sidney Kimmel Comprehensive Cancer Center and Johns Hopkins School of Medicine. “The fewer cancer cells, the better the chance for a successful outcome.”
Screening blood for circulating tumor DNA (ctDNA) through liquid biopsy offers significant promise of improving early detection, he said. Screening using blood samples is easy, minimally invasive, and can detect multiple cancer types. The challenge is identifying tumor DNA in the flood of non-tumor DNA.
Screening with multiple biomarkers is more effective than a single biomarker, Papadopoulos explained. Combining ctDNA with protein biomarkers is far more successful than either biomarker separately. The prospective DETECT A screening study of 10,000 women without known cancer doubled the number of cancers detected by standard-of-care screening alone, including tumors for which there is no standard screen.
The next step is to increase sensitivity without losing specificity, Papadopoulos said. One approach is to add methylation, fragmentomics, aneuploidy, and other genomic/epigenomic elements to existing biomarkers.
“We still need trials to validate screening utility,” Papadopoulos said. “Screening has to be in the target population to avoid spectrum bias and the clinical outlook must be short term. And we need to integrate these multicancer tests into routine screening and management efforts if we are going to reduce the numbers of advanced tumors and improve outcomes.”

We also need to reduce treatment resistance, and not just resistance to on-target effects of radiation, chemotherapy, targeted molecular agents, or immunotherapy, according to Charles L. Sawyers, MD, FAACR, Memorial Sloan Kettering Cancer Center. Clinicians and researchers are seeing resistance evolving through mechanisms that are not related to the therapeutic target.
“We have largely learned the rules for on-target resistance,” Sawyers said. “Next-generation drugs are great, but they place increased inhibitor pressure on a single target. Eventually, they select for off-target escape mechanisms.”
Off-target escape is enabled by genomic alterations such as the loss of RB, TP53, and PTEN that co-occur with alterations to the drug target. These off-target mutations take advantage of lineage plasticity that allow tumor cells to undergo cell state changes and continue to proliferate, Sawyers explained.
In prostate cancer, for example, JAK/STAT and FGFR signaling take advantage of intratumoral heterogeneity to spawn multiple lineage trajectories. Each new trajectory is a potential escape mechanism.
“The ultimate intervene-early strategy is to detect and treat at the precancer stage, but we need a commercial model that creates the necessary incentives,” Sawyers said.
[sub-post-content]
