Opening Plenary Session showcases important breakthroughs across the spectrum of cancer research
During Sunday morning’s Opening Plenary Session: Advancing the Frontiers of Cancer Science and Medicine, an expert panel showcased cutting-edge research that is opening up new frontiers in all areas of cancer research, from basic science and drug discovery to population science and health equity.
The session can be viewed on the virtual meeting platform by registered Annual Meeting participants through July 19, 2023.

Deborah Schrag, MD, MPH, Chair of the Department of Medicine at Memorial Sloan Kettering Cancer Center, discussed the promise and challenges of scaling new cancer screening technologies, including the potential for multi-cancer early detection (MCED) tests to transform cancer screening.
“MCED assays use different molecular methods and combinations of methods to detect cancer from a biospecimen, usually blood, before a tumor becomes symptomatic or lethal,” Schrag said.
MCED tests developed by more than 30 firms are currently in various stages of development and testing. While some early studies are encouraging, Schrag said clinical utility studies are needed to evaluate whether MCED testing reduces cancer-specific mortality — the primary goal of all cancer screening.
“MCED technologies have potential to transform screening and health care delivery,” she said. “Moving forward, we need to take a nimble approach to pragmatic trial design and execution to evaluate this technology. Translation from discovery to clinical to population science and back will be critical for accelerating progress.”

David G. DeNardo, PhD, Professor of Medicine in the Oncology Division at Washington University School of Medicine, reviewed emerging therapeutic strategies to stimulate anti-cancer immunity, such as modulating the systemic impacts of cancer on the immune system and targeting the tumor microenvironment (TME).
“It’s an exciting time to be studying cancer biology and the immune system, and even more exciting is the diversity of immune-based therapies we can bring to bear,” DeNardo said.
While immune-based therapies continue to advance, not all patients benefit from immunotherapies, he said.
“Our challenges now, in 2023, are to identify those patients likely to respond, enhance the durability for patients whose responses are not yet durable, and understand how to leverage the immune system to benefit those patients and cancer types for which we do not yet know how to use the immune system as a therapy to treat their cancer,” he said.

Teresa A. Zimmers, PhD, Professor of Cell, Developmental, and Cancer Biology at Oregon Health & Science University’s Knight Cancer Institute, described important new insight into the complexity of cachexia and its impact on cancer outcomes.
“Cachexia occurs early in many cancers, correlating to aggressiveness, and it predicts survival better than age, stage, or performance status,” Zimmers said. “Additionally, cachexia reduces efficacy of anti-cancer therapies — including surgery, chemotherapy, immunotherapy — and likely causes death through immune compromise and cardiorespiratory failure.”
Zimmers said there’s an enormous need to develop proven therapeutic options for cachexia.
“It’s highly likely that existing therapeutics could be repurposed to treat cachexia now,” she said. “Cancer drives cachexia, but cachexia drives cancer growth, spread, treatment intolerance, and mortality. Cachexia results from specific, targetable mechanisms and, by treating cachexia, we can improve quality of life, length of life, and chance of cure.”
Robert Yarchoan, MD, Chief of the HIV and AIDS Malignancy Branch at the National Cancer Institute, discussed the latest insights and advances in the prevention and treatment of malignancies in patients living with HIV.
The dual setting of cancer and HIV is an area of research that has long been overlooked and understudied, he said. However, recent advances in the understanding of HIV-associated malignancies, such as Kaposi sarcoma and Castleman disease, have highlighted the need for more research.
Before the development and use of combination anti-retroviral therapy, patients living with HIV and cancer often could not tolerate full doses of chemotherapy. Treatment regimens employing lower doses of chemotherapy drugs were used in those patients, usually with relatively low rates of cure. This has changed and, in general, Yarchoan noted that malignancies in patients with HIV are best treated with the standard-dose regimens that would be used in the general population.
However, many clinicians remain reluctant to use immunotherapy to treat patients with HIV due to concerns about safety or potential reactivation of latent HIV. Yarchoan shared recent data demonstrating that such concerns were unfounded.

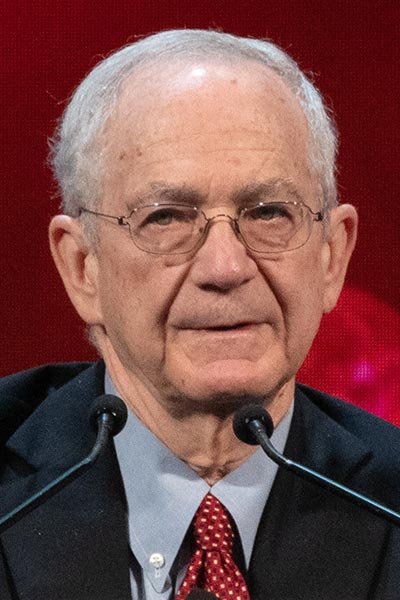
Tomi Akinyemiju, PhD
“While we have made substantial progress in the prevention and therapy of HIV-associated malignancies, they continue to pose a major health problem,” Yarchoan said. “At the same time, our increasing understanding of the pathogenesis of these tumors is leading to novel approaches to their treatment.”
Tomi Akinyemiju, PhD, Associate Professor of Population Health and Global Health at Duke University School of Medicine, discussed the ongoing pursuit of equity at the frontiers of cancer care and the need for both collective responsibility and individual action to effectively address and end cancer racial disparities.
“We need a collective frameshift in how we think about advancing equity and we must recognize that there’s an urgent imperative to advance health equity across the entire translational spectrum,” Akinyemiju said. “And individual action means, be the one to ask the equity question in your domain — who benefits and who is left out? To deliver on the promise of transformative medicine at the frontiers of cancer care, we must urgently address access breakdowns so that everyone benefits.”
More from the AACR Annual Meeting 2025
View a photo gallery of scenes from Chicago, continue the conversation on social media using the hashtag #AACR25, and read more coverage in AACR Annual Meeting News.

