Opportunities in Predictive Oncology Plenary Session defines new approaches to precision medicine
The Opportunities in Predictive Oncology Plenary Session at the AACR Annual Meeting 2025 explored how emerging computational, biological, and clinical methodologies are shaping the ability to predict and personalize cancer treatment for the benefit of patients.
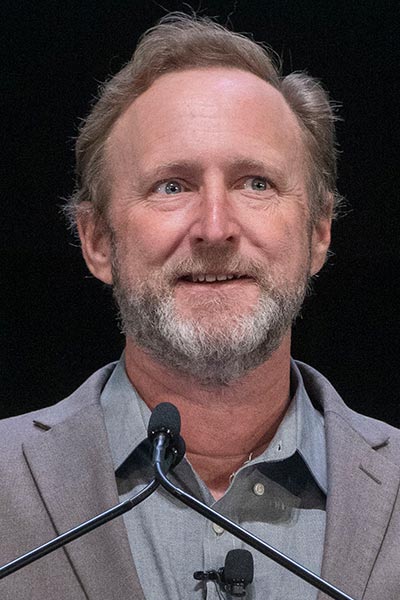
Session chair David W. Craig, PhD, of City of Hope Comprehensive Cancer Center, noted that precision medicine is a cornerstone of the strategy to improve cancer outcomes. “Understanding one patient at a time [and] predicting responses to treatments at the individual level, such as with immunotherapy, remains a critical challenge that involves multiscale, multiomic data with spatial data, longitudinal data, single-cell data,” he said. “Bringing them all together provide[s] new opportunities for decoding and understanding the tumor behavior, the response to therapy, and how to improve outcomes.”
‘Quantum’ cancer therapy at the cellular level

Andrea Califano, Dr, FAACR, of Columbia University, began by sharing the question that has occupied him and colleagues for 20 years: “How is it possible that with an almost infinite number of mutational patterns, you end up having cancer cell states that are rather finite and limited in terms of their characteristics?”
Research has shown that the answer lies in tumor checkpoints, which are master regulators of the cell. Califano revealed that tumor cells’ master regulator modules are limited in number and can combine to give the tumor specific characteristics. “Rather than drugging mutations that are very much upstream of the master regulator modules and that will almost inevitably, within the same tumor mass, have both bypass or alternative mutations that will still feed into that module, maybe what we should do is to drug the module directly,” he said.
Recent work has indicated that treated cells can spontaneously reprogram themselves after initial ablation and that even tumors with the same mutations can occupy different reprogrammable cell states, indicating that tumors can be very heterogeneous at the single-cell level. Algorithms used in conjunction with patient data can help predict in the research setting which combinations of therapies would be effective against a tumor’s specific cell state.
“We don’t have to come up with personalized medicine recipes that are unique to the individual,” Califano said. “We have to come up with personalized recipes that are unique to the actual cell state.”
Multiscale modeling of malignancy

Christina Curtis, PhD, MSc, of Stanford University, focused her talk on the premise that if scientists can make measurements at multiple scales—molecular, cellular, tissue, organismal, and population—they may be able to predict a tumor’s future trajectory. To help patients, they must be able to predict phenotypes related to therapeutic resistance or disease relapse and do it across patients with different underlying disease, she said.
Curtis and colleagues proposed a new model of tumor evolution in which mutations accrue, often in the preneoplastic setting, followed by subsequent neutral growth as the tumor growth dilutes signals of selection. “[This] suggests that malignant potential is specified exceedingly early, [so] might not metastatic potential also be specified early?” she said.
Modeling work has enabled Curtis and others to use lineage tracing methods to determine the underlying clonal dynamics, which they have shown to be reproducible in work with breast cancers. “[With a molecular map of disease] defined based on hormone receptor status, we learned that there are subgroups fueled by chromosomal instability,” she said. “Importantly, this approach also uncovers novel vulnerabilities to target some of these defects.”
Curtis noted that computational biology and related fields now have the tools to pursue rich data capture at diagnosis, at recurrence, throughout the disease course, and even before the onset of overt malignancy.
“I would put forth that with these tools in hand, we can not only develop improved biomarkers, we can better risk stratify,” she said. “We might be able to intercept, and this should certainly inform the approach to therapeutic development.”
Predicting treatment response in TNBC

Marleen Kok, MD, PhD, of the Netherlands Cancer Institute, took the stage next to build on the talk given by Curtis, and provide a clinical perspective on precision immunotherapy and triple-negative breast cancer (TNBC).
Noting that TNBC is the most inflamed breast cancer subtype, Kok said she sees patients with tumors that are 80% or 90% tumor infiltrating lymphocytes (TILs). Adding pembrolizumab (Keytruda) to standard chemotherapy improves overall survival by 5%, but without predictive biomarkers, physicians have no way to know which patients benefit from immunotherapy, she said.
Kok discussed efforts to better understand which patient populations may benefit from anti-PD-1 immunotherapy, with or without chemotherapy. Preliminary clinical trial results showed that tumors with a higher proportion of TILs were more likely to respond to immunotherapy. In these patients, “complete responses to immunotherapy can happen with only a few weeks of immunotherapy without chemotherapy,” she said.
Kok concluded by focusing on patients with metastatic TNBC, saying that treatment with anti-PD-1 immunotherapy can be successful, at least until the patient’s tumor develops acquired resistance. “The literature is quite thin here,” she said. “Studying acquired resistance in patients is difficult because most of the studies are done by pharma with baseline biopsies if biomarkers are presented at all.” She added that obtaining biopsies at diagnosis would be challenging for both clinical trialists and the patients themselves, given the gravity of the diagnosis.
The majority of responding TNBC tumors eventually developed secondary resistance, said Kok. “At baseline, those patients, though, have a more favorable tumor microenvironment, but if you look further, you see that secondary resistance is related to loss of B cells, loss of clonal T cells, and downregulation of the antigen presentation machinery.”
Applying machine learning to predict response

The session’s final speaker, Trey Ideker, PhD, of UC San Diego, focused on predicting drug sensitivity, understanding resistance and progression through multiscale longitudinal data network-based approaches.
In describing the conceptual steps in constructing a cancer genome translator, Ideker emphasized the need for what he called a “middle layer” between inputs and outputs: rational explanations rather than just predictions. He described the goal of constructing molecular maps of cell and tissue organization systematically. “The view of not just single genes, proteins, and mutations, but how those impact larger subcellular machines we think is going to be absolutely key to making forward progress in these precision oncology settings,” he said.
Ideker discussed using machine learning and deep neural networks. “The idea is, can we translate somatic genomic mutations, copy number amplifications, and copy number deletions through the deep learning system to predict the response to a given therapeutic regimen of interest?” he said, adding that one could use the tumor cell map of their choice to train a network. “I think we’re in a rapidly evolving space right now where how you train, starting with which of these datasets and then transitioning to which other datasets, is going to evolve quickly.”
The recording of the full session is available for registered Annual Meeting attendees through October 2025 on the virtual meeting platform.
More from the AACR Annual Meeting 2025
View a photo gallery of scenes from Chicago, continue the conversation on social media using the hashtag #AACR25, and read more coverage in AACR Annual Meeting News.

