Session on drug resistance honors late researcher Joseph R. Bertino, MD, FAACR

The quest to overcome one the biggest challenges in cancer treatment—resistance to therapy—is inextricably linked to Joseph R. Bertino, MD, FAACR.
Bertino, who died in October 2021 at age 91, helped define the mechanisms of action and resistance to one of the most important cancer chemotherapy agents, methotrexate. His groundbreaking work provided the first example of gene amplification as a mechanism of drug resistance.
The AACR honored his legacy Saturday, April 9, by dedicating the Educational Session Drug Resistance: Challenges and Prospects to Bertino’s memory. The session can be viewed on the virtual platform by registered meeting participants through July 13, 2022.
Session chair Sanjay V. Malhotra, PhD, Knight Cancer Institute at Oregon Health & Science University, opened the session with a discussion about designing drugs to target resistance.

SU056, an azopodophyllotoxin small molecule, has been found to inhibit YBX-1, which decreases ovarian cancer cell proliferation. YBX-1 inhibition via SU056 treatment also sensitizes ovarian cancer cells to treatment with the drug paclitaxel, Malhortra explained.
Research suggests the YBX-1 protein influences the function of the translational machinery of RNA.
“If you can target this translational machinery somehow, it could be possible to resensitize cancer cells to the treatment, and that may lead to better outcomes,” Malhortra said.
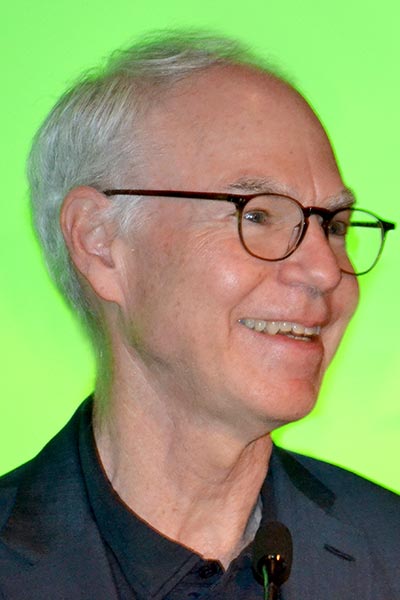
Peter K. Sorger, PhD, Harvard Medical School, discussed the mechanisms of combination cancer therapy in overcoming intrinsic and acquired drug resistance.

The vast majority of cancers, both liquid and solid, are treated with combination therapies, yet the existing therapies nearly always exhibit independent drug action rather than additivity or synergy, explained Sorger.
The Frie Independence Model, a concept dating back 60 years, explains the progression-free survival (PFS) benefit in most approved clinical combinations of cancer drugs, but particularly in immune checkpoint inhibitors, he said. The likely but as-yet unproven explanation is too much patient-to-patient variability to achieve double response.
“What we like is when we get additivity in curative therapies. That would be our goal,” said Sorger, adding that patient response by PFS or overall survival improves significantly when that additivity is achieved. “It’s a pretty big goal, and we think this is going to take more accurate patient stratification.”
- More Here: To read about Sorger’s research on independent drug action, visit AACR’s blog Cancer Research Catalyst
Tissue imaging is one pathway toward that goal that Sorger expects to deliver in the coming years.
“Those types of imaging assays are typically executed as laboratory development tests in hospitals, so there’s actually a quick route to clinical translation,” he said.
Former AACR President Charles L. Sawyers, MD, FAACR, Memorial Sloan Kettering Cancer Center, concluded the session with a presentation about shifting the mechanisms of acquired resistance to therapy. Next-generation, on-target inhibitors have proven effectiveness in improving patient outcomes, he said.
“We can make very precise, potent inhibitors of the primary driver target, and we can get predictable mechanisms of relapse now,” said Sawyers, but cautioned that this approach requires ongoing development to keep up with new, on-target escape mechanisms.
“We’re converging to a set of small core developmental pathways that offer some optimism that we could come after them therapeutically,” he continued.
“Increased inhibitory pressure on a single target will eventually select for off-target escape mechanisms,” added Sawyers, listing two notable exceptions: gastrointestinal stromal tumors and chronic myeloid leukemias. This escape is enabled by co-occurring genomic alterations that allow tumor cells to undergo cell-state changes such as lineage plasticity.
[sub-post-content]
