Special symposium commemorates 40th anniversary of KRAS discovery
The cancer world changed in 1982 when three labs, working independently, identified the first confirmed human oncogene, RAS, and cloned three variants: HRAS, KRAS, and MRAS.

The Kirsten rat sarcoma viral oncogene homolog (KRAS) is mutated in about 25 percent of all human tumors, but it took another three decades of research to transform KRAS from the most attractive cancer target to a druggable protein when sotorasib was approved by the U.S. Food and Drug Administration in 2021.
“1982 was more than the confirmation that oncogenes are real,” said Patricia M. LoRusso, DO, PhD (hc), Yale University School of Medicine and Yale Cancer Center. “The developments of 1982 were a crucial step toward our current understanding of cancer as a complex interplay between different types of genetic lesions.”
LoRusso chaired the symposium KRAS Anniversary Session: Novel Mechanisms for Targeting KRAS on Monday, April 11. The session can be viewed on the virtual platform by registered meeting participants through July 13, 2022.
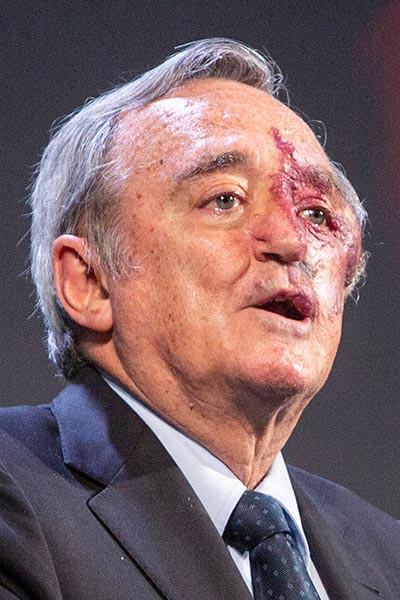
The search for human oncogenes began in 1976 when a paper published in Nature described the first vertebrate genes that could be transformed by mutation into oncogenes, recalled Mariano Barbacid, PhD, Spanish National Cancer Research Center. Barbacid’s lab identified HRAS in 1982.
Cancer researchers quickly realized that HRAS, NRAS, and KRAS were all potential, if elusive, drug targets. Barbacid suggested an alternative approach. Instead of inhibiting KRAS, a biochemically difficult task, it may be more effective to target KRAS oncoprotein expression, he reasoned.
“When you inhibit an oncogene, you can expect resistance to develop quickly,” he said. “If you degrade the oncoprotein, you eliminate KRAS expression. If you eliminate the oncoprotein, there is not going to be resistance.”
Multiple mouse models support the degradation strategy to target KRAS, Barbacid continued. Ablating KRAS expression both avoids resistance and reduces toxicity in preclinical models.
“KRAS degradation will be a better therapeutic strategy than KRAS inhibition,” he predicted.
For now, KRAS inhibition is the therapeutic approach approved by regulators. RAS proteins activate the MAP kinase pathway leading to cell proliferation, migration, and survival.
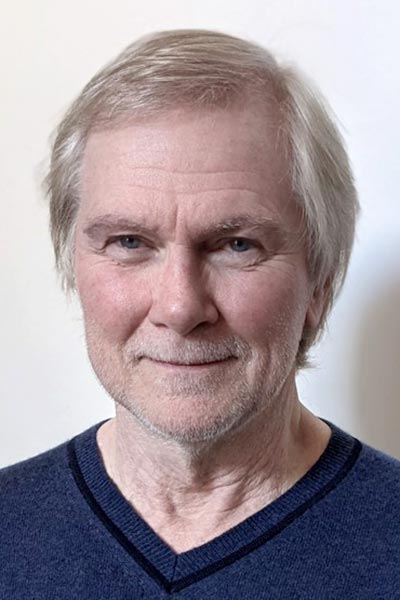
“In cells with oncogenic RAS, they regulate abnormal cell proliferation and survival,” said Frank McCormick, PhD, University of California, San Francisco. “In normal cells, RAS is very well regulated. In tumor cells, RAS is always ‘on’ instead of only being active for specific steps in the cell cycle. The sustained activation of MAPK leads to transformation.”
It’s still not entirely clear how RAS proteins function, but a single amino acid variation turns normal RAS into an oncogene. It took years of painstaking biochemical work to identify a potential target on the mutated gene.
“The G12 substitution is a disease-relevant mutant,” said Kevan M. Shokat, PhD, University of California, San Francisco, who was the first to successfully drug KRAS in 2013. “Cysteine is the third-most frequently altered amino acid and forms an unbreakable bond that is tumor-specific. No normal tissue has cysteine at the G12 position.”
Early ligands failed to bind well to an initial pocket, but a second pocket has been more successful, Shokat continued. Some molecules are active in vitro but not in animals. The first molecule active in vivo was identified in 2018.

Different research teams have identified different agents that target KRASG12C, including sotorasib and adagrasib. Both use a β-lactone warhead that can be tuned, which Shokat said could offer additional therapeutic opportunities.
Sotorasib and adagrasib both show good antitumor activity but with very different pharmacokinetics, LoRusso explained.
Sotorasib, which is in clinical use, has a half-life of 5.5 hours, a recommended dose of 960 mg daily, and nonlinear pharmacokinetics.
Adagrasib, still in trials, has a half-life of 24.7 hours, a recommended dose of 600 mg BID, and linear pharmacokinetics.
Sotorasib shows treatment response at all doses and disease control ranging from 88.1 percent in non-small cell lung cancer (NSCLC) to 73.8 percent in colorectal cancer (CRC). A two-year analysis of CodeBreak 100 reported during the AACR Annual Meeting 2022 showed 12.3 months median duration of response with 50.6 percent of responders in remission for at least 12 months. Overall survival was 12.5 months and two-year survival was 32.5 percent.
Adagrasib shows good response in NSCLC and CRC, both as monotherapy and in combination with cetuximab, LoRusso reported.
So why are responses to KRASG12C inhibition not deeper and more prolonged?
Patients in all trials were heavily pretreated, LoRusso noted, and likely had co-mutations that are not targeted.
“We know there is significant crosstalk with other pathways we are not targeting with immunotherapy,” she said. “And sotorasib has a short half-life, raising questions about whether drug levels remain high enough to deter the development of resistance. We have to ask about combination therapy.”
Preclinical data for combination therapy with EGFR inhibitors, MEK inhibitors, mTOR inhibitors, HER inhibitors, and SHP2 inhibitors are promising, LoRusso said, and clinical response rates to adagrasib plus cetuximab are better than response rates to adagrasib alone.
Early-phase combination trials of sotorasib are underway. A phase I study of sotorasib/afatanib showed very good tumor response with a decrease in target-lesion size in 83 percent of patients, but toxicity is a problem. Nearly half of the patients in a high-dose arm had dose modification due to adverse events and 17 percent discontinued treatment.
“Many of the G12C inhibitors are very active, but not as active as we had hoped,” LoRusso said. “We are still looking for a cure.”
More from the AACR Annual Meeting 2025
View a photo gallery of scenes from Chicago, continue the conversation on social media using the hashtag #AACR25, and read more coverage in AACR Annual Meeting News.

