Researchers report first disclosures of 12 novel cancer agents
//
Estimated Read Time:

The AACR Chemistry in Cancer Research working group, which is chaired by Mary M. Mader, PhD, organized three special sessions at the Annual Meeting that featured first disclosures on the discovery, structure, and mechanism of action of 12 novel cancer agents that have recently entered into phase I clinical trials or will do so in the next few months.
The first two sessions took place Sunday, April 16, followed by a final session on Monday, April 17. All three sessions can be viewed on the virtual meeting platform by registered meeting participants through July 19, 2023.
New Drugs on the Horizon: Part 1
ABBV-319: A first-in-class glucocorticoid receptor modulator (GRM) agonist ADC for the treatment of B-cell malignancies
James Purcell, PhD, of AbbVie Inc., reported study findings on ABBV-319, a multimodal CD19-targeting antibody-drug conjugate (ADC) with a glucocorticoid receptor modulation (GRM) agonist that is more potent than systemic prednisolone or dexamethasone in clinical use, he said. Glucocorticoids have proven single-agent activity on B-cell malignancies but carry a high burden of serious and debilitating adverse events.

“If we had a highly potent steroid and delivered it via ADC, we would be able to get increased activity while also improving the tolerability of these agents,” Purcell said. The therapy his team developed consists of a glucocorticoid receptor agonist and an antibody targeting CD19, which is functionally required for the growth of B-cell malignancies even after prior CD19-targeted agents.
ABBV-319 is highly efficacious in multiple cell line xenograft and patient-derived xenograft (PDX) models of B-cell malignancies, Purcell reported. Ten of 10 diffuse large B-cell lymphoma PDX models showed tumor-growth inhibition, with nine models showing tumor regression with a single dose. Efficacy was seen in both germinal center B-cell (GCB) and non-GCB models from patients with recurrent disease.
Purcell and colleagues have completed preliminary studies of the ADC in a non-human primate model with no severe toxicities. They recently started a phase I clinical trial in patients with relapsed or refractory B-cell malignancies.

CTX112 and CTX131: Next-generation CRISPR/Cas9-engineered allogeneic (allo) CAR T cells incorporating novel edits that increase potency and efficacy in the treatment of lymphoid and solid tumors
First-generation allogeneic (allo) CAR T-cell therapies against CD19 and CD70 have shown encouraging efficacy in clinical trials of B- and T-cell lymphomas and renal cell carcinoma (RCC). But T-cell exhaustion can result in decreased efficacy and loss of response, especially in patients with a high tumor burden.
Jon Terrett, PhD, of CRISPR Therapeutics, and colleagues screened for gene knockouts that could improve the potency of allo CAR T cells. They found a pair of genes, Regnase-1 and the transforming growth factor beta receptor 2 (TGFBR2), that, when knocked out, produced cells with improved cell-killing and functional persistence, resistance to environmental suppression, and memory preservation. These discoveries led to the development of two next-generation allo CAR T cells: CTX112 (anti-CD19) and CTX131 (anti-CD70).
CTX112 increased survival in CD19+ Nalm6-Luciferase leukemia models compared to CAR T-cell controls, Terrett reported. In a cell xenograft model, a single dose of CTX131 produced complete regression of NCI-H1975 lung cancer and prevented tumor growth upon rechallenge with both ACHN and Caki-2 RCC cells, he added.
“These new edits, I think, will allow us to go after tougher indications,” Terrett said. “We’re seeing hints now of solid tumor activity. I think with these new edits, we can push the envelope even further.”
Discovery of ARV-766, an androgen receptor degrading PROTAC® for the treatment of men with metastatic castration-resistant prostate cancer
Prostate cancer is the second-leading cause of cancer death in men in the U.S., and while therapeutic approaches targeting the androgen/androgen receptor (AR) axis are effective initially, castration-resistant prostate cancer (CRPC) eventually appears.
Proteolysis-targeting chimera (PROTAC®) drugs target disease-causing proteins for degradation, eliminating them rather than simply inhibiting them, explained Lawrence B. Snyder, PhD, of Arvinas Inc. “This has a real potential for being able to degrade very difficult proteins and attack very difficult disease states,” he said.
ARV-766 is a second-generation PROTAC®-targeting the ligand binding domain mutation L702H, one of the most common AR mutations in men with advanced prostate cancer. The mutation typically emerges as a result of antiandrogen therapy and drives resistance. ARV-766 degrades wildtype AR as well as L702H and other clinically relevant AR mutants that develop and expand after antiandrogen treatment. The agent is based on ARV-110 (bavdegalutamide), a first-generation PROTAC® that is currently in phase II trials.
In non-castrated mice, ARV-766 reduced tumor growth and prostate-specific antigen (PSA) levels significantly better than the antiandrogen enzalutamide. “This is a higher bar to clear than the castrated setting, because these mice have endogenous levels of circulating androgens that ARV-766 has to compete against,” Snyder said.

BAY 2965501: A highly selective DGKζ inhibitor for cancer immunotherapy with first-in-class potential
The tumor microenvironment (TME) can suppress T-cell function, reducing the activity of anti-PD-L1 and other immunotherapeutic approaches. Diacylglycerol (DAG) plays a key role in T-cell activation through downstream T-cell receptor signaling. Diacylglycerol kinase zeta (DGKζ) modulates the DAG pathway to provide negative feedback on T-cell activation. DGKζ-deficient T cells are hyper-reactive and show enhanced effector function. DGKζ also provides negative feedback to natural killer (NK) cell activation.
A new DGKζ inhibitor, BAY 2965501, reduces T-cell exhaustion and increases T-cell proliferation/activation to re-establish effector function and increases NK-cell activation, reported Dennis Kirchhoff, PhD, of Bayer AG. BAY 2965501 does not have any direct antiproliferative effects on tumor cells but has a strong dose-dependent effect on T cell-mediated tumor cell killing in melanoma cells and a mouse testicular teratoma model, Kirchhoff noted. The agent also improves NK cell-mediated antitumor activity.
Combining BAY 2965501 with anti-PD-L1 immunotherapy significantly increases antitumor activity compared to either agent in monotherapy, he added.
“Our data clearly show a complementary mode of action between a selective suppressive ligand, like PD-L1, and enhancing the signal, borne by DGKζ inhibition,” Kirchhoff said. “Upon combination, we see clear additive effects.”
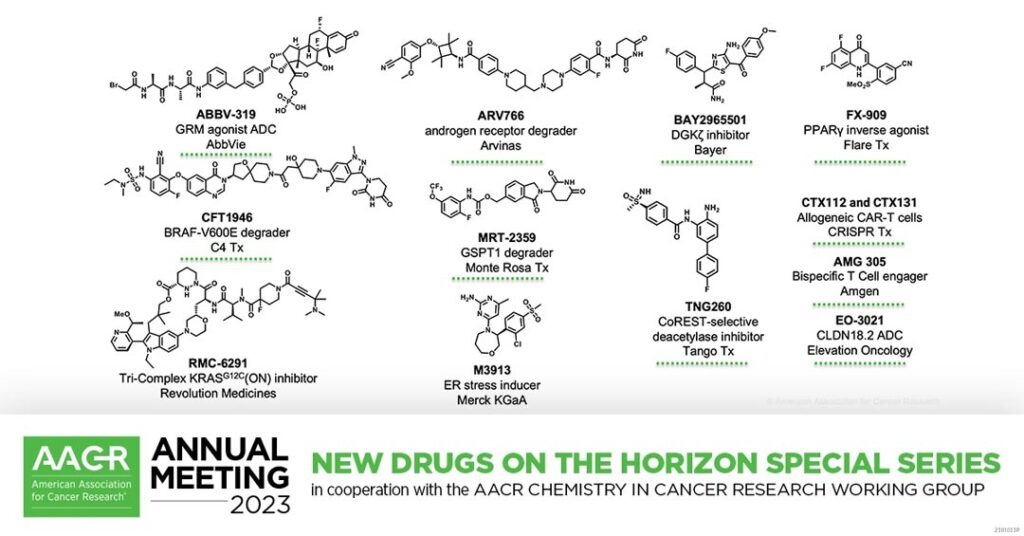
New Drugs on the Horizon: Part 2
The discovery and characterization of CFT1946: A potent, selective, and orally bioavailable degrader of mutant BRAF for the treatment of BRAF-driven cancers
Mutated BRAF kinase is seen in about 8 percent of human tumors, including 60 percent of thyroid and melanoma tumors and 10 percent of lung adenocarcinomas. Current BRAF-targeted agents are highly effective, but nearly all patients progress due to resistance. The most common mutation is BRAF-V600E, a protein kinase in the MAPK pathway that promotes cell proliferation and survival.
Inhibiting BRAF causes a paradoxical activation of wildtype RAF by promoting formation of a RAF/BRAF dimer, explained Yanke Liang, PhD, of C4 Therapeutics. A novel agent, CFT1946, uses a degrader to overcome the limitations of current BRAF-inhibiting approaches. Degraders avoid the paradoxical activation of RAF and can target specific BRAF mutations while sparing wildtype BRAF, he said.
CFT1946 is an orally bioavailable bifunctional degradation activating compound (BiDAC) that targets the BRAF-V600E mutation. The agent causes potent inhibition of MAPK signaling and loss of viability in BRAF-V600E cells in vitro and in vivo but has no effect on wildtype BRAF cell-growth or MAPK signaling. The compound is highly active in a BRAF-V600E/NRAS-Q61K cell xenograft model, a model of clinical resistance to BRAF inhibitors, as both a single agent and in combination with a MEK inhibitor.
“Based on the preclinical profile, CFT1946 is currently being evaluated in phase I clinical trials,” Liang said.

AMG 305, a dual targeting BiTE® molecule with selective activity for solid tumors that co-express CDH3 and MSLN
Bispecific T-cell engagers (BiTE®) are a familiar targeted immunotherapy approach, but clinical development of these agents has been challenging, especially in solid tumors. Few tumor-surface antigens are tumor-specific, and even low levels of expression in normal tissue can lead to on-target, but off-tumor activity.
One solution is a dual-targeting BiTE®, in which both targets are expressed on tumors, but normal tissue expresses just one or neither of the targets, explained Elizabeth Pham, PhD, of Amgen. “Dual-targeting BiTE molecules have the potential to improve the therapeutic index of tumor antigens that have some normal tissue expression,” she explained.
Pham and colleagues developed the BiTE® AMG 305, which requires the engagement of both CDH3 and MSLN to produce potent antitumor activity. “The proposed mechanism of action for dual-targeting BiTE® molecules is an avidity-driven approach to preferentially target tumor cells that are double-positive for CDH3 and MSLN, with limited activity against normal cells that express only one or the other target, but not both,” she said.
AMG 305 showed dose-dependent antitumor activity in cell xenograft models and was well tolerated in cynomolgus monkey studies at exposure levels well above the predicted human efficacious doses, Pham reported. The agent induces potent cytotoxicity against tumor cells that co-express CDH3 and MSLN, which were selected as targets based on the co-expression seen in lung and other solid tumor types, but only rarely in normal tissue, she explained.

Discovery of RMC-6291, a tri-complex KRASG12C(ON) inhibitor
RAS mutations resulting in excessive RAS signaling drive about 30 percent of human cancers. The KRASG12C mutation is a recognized target, but currently approved agents target the inactive conformation of KRAS (KRAS(OFF)) rather than the active form (KRAS(ON)).
“RAS mutations are drivers in nearly a quarter of a million new cancer cases per year,” said Jim Cregg, PhD, of Revolution Medicines. “We believe that targeting the active form of KRASG12C could provide improved clinical benefit to these patients.”
RMC-6291 is a KRASG12C(ON) inhibitor that forms a tri-complex with KRASG12C(ON) and cyclophilin A to quickly suppress RAS pathway activity and drive profound tumor regression, Cregg reported.
“RMC-6291 is well tolerated and highly active in preclinical studies in vivo,” Cregg said, noting strong tumor regression and high response rates in cell xenograft models of non-small cell lung cancer (NSCLC).
Pharmacokinetic studies showed that RMC-6291 blocks KRASG12C activity more completely and rapidly than the RAS(OFF) inhibitors sotorasib and adagrasib. “We attribute this to the fact that they have to wait for the OFF state, which is limited by the rate of GTP hydrolysis of KRASG12C,” Cregg said. In a mouse clinical trial using 25 KRASG12C NSCLC models, RMC-6291 elicited a better response rate and progression-free survival than adagrasib.

Discovery of FX-909, a first-in-class inverse agonist of the peroxisome proliferator-activated receptor gamma (PPARG) lineage transcription factor, to potentially treat patients with the luminal subtype of advanced urothelial cancer (UC)
The treatment landscape of advanced urothelial cancer (UC) has improved over the last decade, but metastatic UC still has one of the worst recurrence rates of any cancer. Two-thirds of advanced UC is luminal and is characterized by overexpression of the urothelial lineage-defining transcription factor peroxisome proliferator-activated receptor gamma (PPARG).
A new agent, FX-909, is a first-in-class covalent PPARG inverse agonist. “The activity of FX-909 is on-target, it is predictable, it is gradual in its onset, and it is reversible,” said Robert J. Simms III, PhD, of Flare Therapeutics. The agent potently suppresses the growth of bladder cancer cells in animal models at doses as low as 0.03 mg/kg, equivalent to the projected starting dose for the phase I clinical trial, Simms said.
“We’re incredibly excited to move FX-909 into the clinic, with the ultimate objective of providing patients with lethal muscle-invasive bladder cancer new options,” he continued.
New Drugs on the Horizon: Part 3

M3913 induces the maladaptive unfolded protein response through a novel mechanism resulting in strong antitumor activity
Exposure to hypoxia and other stressors can induce the unfolded protein response, which can improve cell survival. Inducing an exaggerated and maladaptive unfolded protein response in the endoplasmic reticulum (ER) can instead cause cell death and is therefore a novel and potentially effective therapeutic paradigm in cancer treatment.
“The maladaptive protein response is basically a mechanism by which the cell makes a cell fate decision when protein stress becomes so strong and excessive that it shifts from repairing the stress to inducing cell death,” explained Ralph Lindemann, PhD, of Merck KGaA.
A novel agent, M3913, induces transient calcium efflux from the ER, triggering bona fide ER stress signaling via the protein Wolframin 1, which is expressed in many human cancers, Lindemann reported. In vitro and in vivo multiple myeloma and NSCLC models showed that M3913 can mediate long-lasting tumor control as a single agent. In vitro studies suggest good potential for M3913 combination therapy with a variety of chemotherapy agents, multiple signaling pathway inhibitors, and immunotherapeutic agents, Lindemann said.
Lindemann also mentioned that his team has seen preliminary markers of efficacy in other solid-tumor indications, including triple-negative breast cancer. “We believe M3913 is a potential first-in-class therapy,” Lindemann said.

Discovery of MRT-2359, an orally bioavailable GSPT1 molecular glue degrader, for MYC-driven cancers
MYC gene family transcription factors are key cancer-dependent genes and are among the most dysregulated oncogenes in human cancer. C-MYCs, N-MYCs, and L-MYCs are considered undruggable by classic methods, but because MYC-driven cells are addicted to protein translation, they are vulnerable to loss of the translation termination factor GSPT1.
A novel molecular glue degrader (MGD), MRT-2359, was designed for slower, more targeted degradation of GSPT1 compared to other MGDs. It is highly selective for MYC-driven cells and neuroendocrine (NE) cell lines and preferentially impairs protein synthesis in tumor cells with high MYC expression, reported Owen B. Wallace, PhD, of Monte Rosa Therapeutics.
The differential effect of MRT-2359 in MYC-high versus MYC-low models was applicable in prostate, NSCLC, small-cell lung cancer (SCLC), and NE cell lines, Wallace said. He explained that MRT-2359 abrogates protein synthesis preferentially in MYC-high cells, leading to downregulation of MYC transcriptional output, a mechanism that is applicable to C-MYC, N-MYC, and L-MYC.
Preclinical studies in PDX models show a dose-dependent decrease in tumor size in MYC-high NSCLC and SCLC, Wallace added.
“Our compound is currently in a phase I clinical trial; it’s in the dose escalation portion currently,” Wallace said. “We’re enrolling patients with NSCLC or SCLC, high-grade neuroendocrine tumors, N- or L-MYC amplified solid tumors, and diffuse large B-cell lymphoma.”

EO-3021: An antibody drug conjugate targeting CLDN18.2 expressing cancers
Claudin 18.2 (CLDN18.2) is part of a family of tight junction membrane proteins. In normal tissue, CLDN18.2 expression is restricted to the gastric mucosa with basolateral localization, where it acts to prevent gastric leakage. CLDN18.2 is overexpressed in gastric, pancreatic, esophageal, ovarian, lung, and other tumor types, and there are no approved therapies targeting CLDN18.2-expressing tumors.
“One unique aspect is, at least in respect to gastric cancer, CLDN18.2 doesn’t seem overlap much with HER2 or PD-L1, for which they have agents in gastric cancer that are standard of care,” said David Dornan, PhD, of Elevation Oncology. Dornan added that CLDN18.2 is expressed in millions of tumors globally—77 percent of gastric adenocarcinomas, 78 percent of esophageal adenocarcinomas, up to 80 percent of pancreatic cancers, 24 percent of ovarian cancers, and 6 percent of lung adenocarcinomas.
Dornan and his colleagues designed an ADC, EO-3021, with the potential to selectively target and kill CLDN18.2-expressing cancer cells. EO-3021 induces apoptosis in CLDN18.2-expressing tumor cells by arresting the cell cycle in G2/M. It produces tumor regression with a single dose across low, medium, and high CLDN18.2-expressing cells in pancreatic, gastric, and lung cancer cells and xenograft models and shows good bystander effect on nearby CLDN18.2-negative tumor cells, he added.
EO-3021 outperforms gemcitabine in animal models with manageable toxicities. A case study from a non-U.S. phase I trial in recurrent metastatic gastric cancer showed 66.7 percent reduction in the target lesion with response continuing for at least 11 months, he said.

TNG260: A novel, orally active, CoREST-selective deacetylase inhibitor for the treatment of STK11-mutant cancers
STK11-mutant cancers are resistant to anti-PD-1/anti-PD-L1 targeted therapy as tumors develop immune evasion. In KRAS-mutant lung cancers, overall survival after treatment with anti-PD-1/anti-PD-L1 agents is 17.3 months for STK11 wild type and 6.2 months for STK11-mutant tumors. About 15 percent of NSCLC tumors have loss-of-function mutations to STK11.
A novel agent, TNG260, reverses immune evasion caused by STK11 loss-of-function mutations, reported Leanne G. Ahronian, PhD, of Tango Therapeutics. The agent selectively inhibits the activity of the deacetylase complex CoREST, resulting in transcriptional reprogramming of STK11-mutant tumor cells. The transcriptional reprogramming alters tumor-cell cytokine secretion, which improves the recruitment of cytotoxic T cells and markedly reduces recruitment of suppressive Treg cells.
Combining TNG260 and anti-PD-1 therapy reduced tumor growth better than either agent alone in a cell xenograft model of colorectal cancer and completely regressed tumors that were re-implanted.
“We see a shift in T-cell effector activity, increases in antigen presentation, and increases in PD-L1 levels,” Ahronian said. “Taken together, this fuels the antitumor efficacy we see with the combination of TNG260 and anti-PD-1 in our STK11-deficient models.”




